By Santa J. Bartholomew M.D. FAAP, FCCM
See Corresponding Case Study: PARDS
ARDS is an acute lung injury that can be triggered by direct injury to the lung, such as pneumonia, aspiration, near-drowning or burn/smoke injury, trauma or by an extrapulmonary process, such as sepsis, drug overdose, acute pancreatitis, or cancer. This definition excludes lung issues secondary to cardiac disease and neonatal respiratory failure. PARDS manifests as lung inflammation and edema in the alveolar spaces, causing profound hypoxemia. From this acute phase of inflammation, it can progress to a more chronic and fibrotic phase, causing lifelong breathing problems.
The Pediatric Acute Lung Injury Consensus Conference (PALICC) in 2015 provided consensus data and opinions on the definitions and therapeutic treatments for PARDS based on the available literature; this was then updated in 2023. It serves as the guideline for the standard of care for treating ARDS in children.
Diagnostic Criteria
Diagnostic criteria for PARDS according to PALICC: the presence of hypoxia and new chest infiltrate occurring within seven days of a known insult. Hallmarks of ARDS include hypoxemia associated with decreased lung compliance, increased breathing work, and impaired gas exchange. Hypoxemia can be calculated from the A-a gradient: A-a gradient = PAO2 – PaO2 = {FiO2 (Patm – PH2O) – PaCO2/0.8} – PaO2 or the FiO2/PaO2 gradient.
The low oxygen in blood results from areas of intrapulmonary shunt and ventilation-perfusion mismatch. Strategies for therapy are aimed at ameliorating these problems while trying not to cause secondary volutrauma or barotrauma to the lung.

ARDS is an acute lung injury that can be triggered by direct injury to the lung, such as pneumonia, aspiration, near-drowning or burn/smoke injury, trauma or by an extrapulmonary process, such as sepsis, drug overdose, acute pancreatitis, or cancer.
Treatment is Multi-Layered
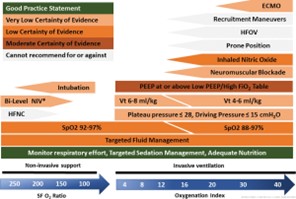
- Non-Invasive Ventilation: used early in the disease in methods such as HHFNC (heated high flow nasal cannula), BiPAP, and CPAP and can be used when adequate oxygenation can be achieved within the first few hours of therapy.
- Invasive Ventilation: When oxygenation is not improving with these methods, placing an endotracheal tube to provide other more sophisticated methods for getting oxygen across the lung membranes must be employed such as PEEP, prone positioning, different strategies of ventilation such as APRV (airway pressure release ventilation) or trials of other types of ventilation such as High-Frequency Jet Ventilation (HFJV) and High-Frequency Oscillatory Ventilation (HFOV).
- ECMO: In extreme cases, ECMO can be utilized as a lifesaving method. Numerous studies associate ECMO with improved survival although PARDS survival is lower than their neonatal counterparts.
- Good nutrition
- Sedation and/or paralysis
Surfactant and Nitric Oxide have been used in ARDS with mixed results in children and are not currently recommended by the PALICC.
Prognosis
Moderate to severe PARDS has high morbidity and mortality in PICU particularly in children with multiple organs failing.
References
Recent Advances in Pediatric Acute Respiratory Distress Syndrome (PARDS). Hough,R. Curr Pediatr Rep (2017) 5:228–236
Executive Summary of the Second International Guidelines for the Diagnosis and Management of Pediatric Acute Respiratory Distress Syndrome (PALICC-2) Pediatric Critical Care Medicine 24(2):p 143-168, February 2023
Pediatric ARDS Chiefetz,I. Respiratory Care June 2017, 62 (6) 718-731
Pediatric Acute Respiratory Distress Syndrome: Medscape Updated: May 31, 2023 Prashant Purohit, MD




