By Santa J. Bartholomew M.D. FAAP, FCCM
Meningitis is the medical word for an infection or inflammation in the skin surrounding the brain and spinal cord. This can be a life-threatening disease in all age groups although the types of bacteria that cause meningitis differ based on age. Meningitis in all age groups can cause permanent damage to the brain and the nerves from the brain; causing hearing loss, mental retardation and other neurologic issues, and even death if not diagnosed and treated quickly.
Table 1: Organisms Causing Meningitis
Blood Brain Barrier
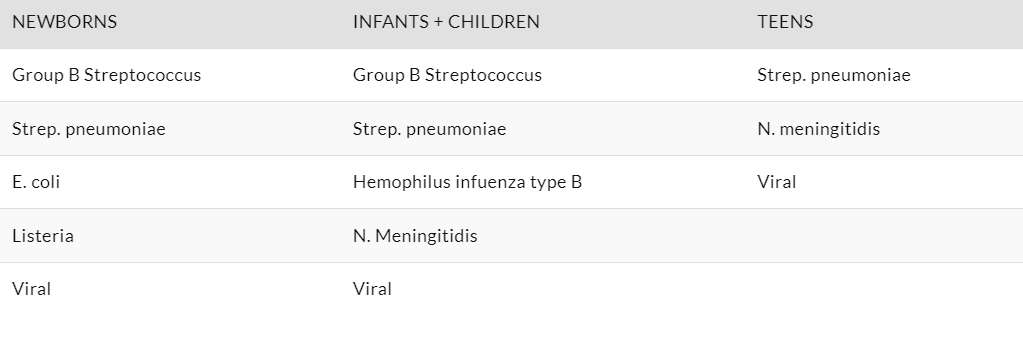
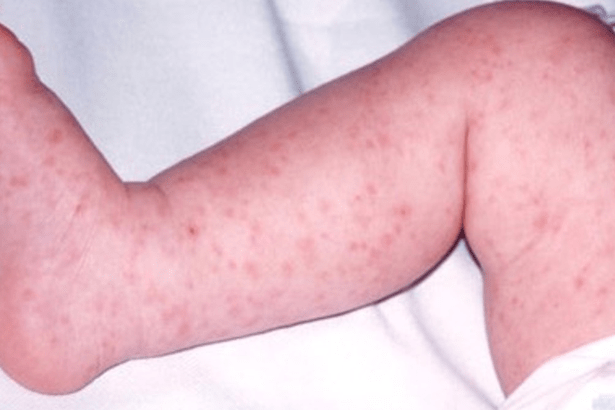
Figure 1: Rashes Associated with Meningitis


When seen in the Emergency Department children often have high white counts (white cells are the infantry of the immune system) as the different types of white cells are released into the bloodstream and have different ways of killing and controlling viruses and bacteria. Although this is enormously helpful to fighting infection it can also injure the brain cells engulfed in the infection and make swelling in the brain and this swelling can decrease blood flow to the brain by compressing blood vessels into the skull and make brain injury worse. In infants there are times when the white cells are very low portending that the child is overwhelmed by infection and at more risk of dying without rapid intervention.
It is vital when a child is brought to the ED that labs are obtained quickly, a diagnosis is made with all possible haste, and antibiotics are started. This all should occur concurrently with checking the child’s ability to breath and swallow and if they are not, then taking control of their airway. Also, treating things like low blood sugar and seizures aggressively as they can injure the brain further.
Besides antibiotics and in some types of meningitis the occasional use of steroids all care is supportive care.
The brain is extremely fragile. It has no alternate way to make energy if there is no glucose in the blood or if blood does not get to and feed the brain. It exists within a fixed space, the skull, so there is limited space for swelling before the brain is injured irreversibly by swelling. Anything that increases the brain’s metabolic demands like fever and seizures can make the outcome worse. So, during the first days of infection, all support is focused on keeping enough sugar in the blood, stopping or controlling seizures, supporting blood pressure to keep adequate blood flow to the brain and controlling swelling.
Healthcare providers will look at the brain by CT initially and intermittently to carefully watch brain swelling depending on how alert the child is and if they are having seizures or not. They should carefully monitor for seizures and treat them aggressively. Mortality for bacterial meningitis in infants can be as high as 20% and 10-12% in older children. But in addition to death meningitis is fraught with difficult consequences: subdural abscesses, hearing loss, hydrocephalus
Finally, meningitis can often be accompanied by overwhelming sepsis in which there is a large burden of circulating bacteria. This prompts a large inflammatory response to fight the toxins released by bacteria. But this can cause high fevers and high HR as well as low blood pressure and organ failure further complicating the supportive goals of protecting the brain.
The key to protecting the brain from injury is quick diagnosis and quick treatment.




