By Santa J. Bartholomew M.D. FAAP, FCCM
See Corresponding Case Study: Hypoxic Ischemic Encephalopathy (HIE)
What is Hypoxic Ischemic Encephalopathy (HIE)?
HIE is a brain injury that occurs from impaired oxygen delivery to the brain (hypoxia) or poor blood flow to the brain (ischemia). This can occur as a result of many things including:
- Impaired gas exchange of oxygen and carbon dioxide
- Lack of nutrients such as glucose
- Metabolic acidosis
Pathophysiology:
The injury to the brain occurs in two phases:
Phase I: The initial injury itself such as catastrophes surrounding birth, cardiac arrest, respiratory arrest, drowning. Any event in which the brain lacks adequate oxygen or blood flow. This initial injury sets in motion a series of chemical processes in the brain that can lead to cell death (necrosis).
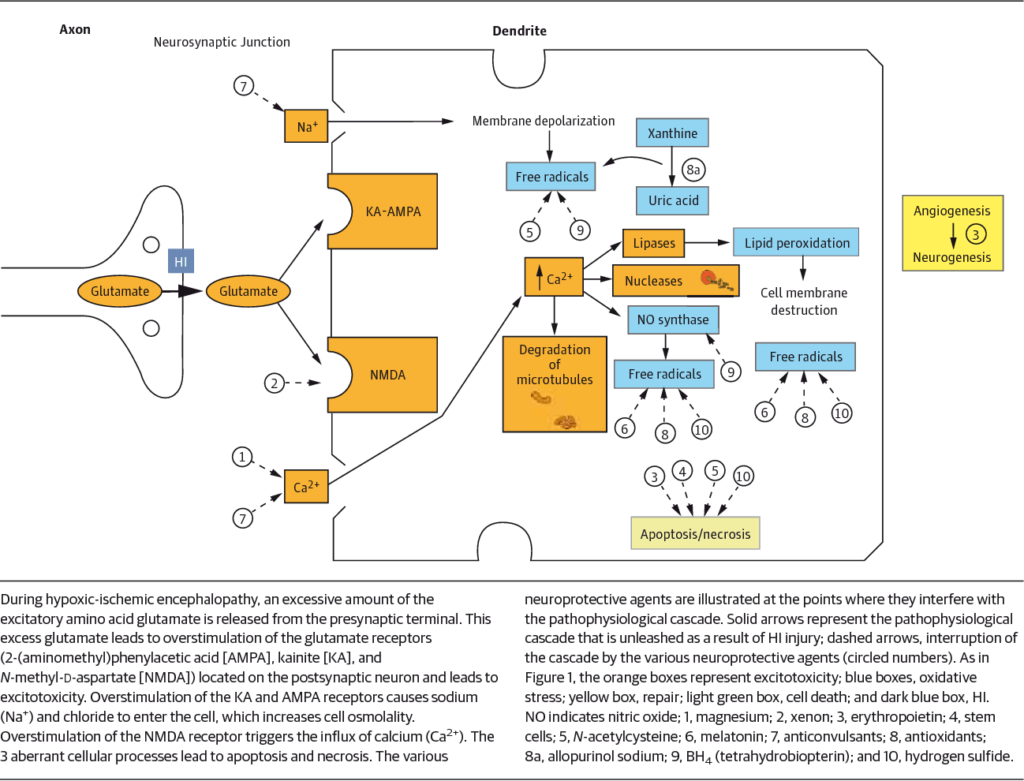
JAMA Pediatrics 2015
Phase II: This phase is more significant than Phase I in that this is the phase in which all therapy is focused and in which small changes in patient status can injury the brain further in cataclysmic ways. This phase begins at 12-36 hours from initial injury can last las long as 14 days. During this phase the inside powerhouse of the brain cell (the mitochondria) begin to fail, the cells in the brain swell and die and when they do they release free radicals and other chemicals that can injure cells around them. All of our therapies are directed at minimizing these secondary injuries.
Neonatal Risk Factors for HIE:
- Umbilical cord issues: occlusion or compression, knotted cord, nuchal cord around infants neck during delivery, oligohydramnios and polyhydramnios
- Placental complications or anything that impairs blood flow through the placenta, placental abruption, ruptures vasa previa, preeclampsia, infection intrapartum hemorrhage, uterine rupture.
- Birth injuries: cephalopelvic disproportion (the head will not fit through the birth canal), shoulder dystocia, improper use of forceps or vacuum extractor, thick meconium aspiration.
Signs and symptoms:
- Stupor or coma
- Seizures
- Lethargy
- Bradycardia and/or agonal breathing
Treatment:
Cooling: is the mainstay of therapy for the best outcomes in injured infants and children.
- Achieving core temperatures 33-34 Celsius: prevents delayed cell death in phase II.
- It also slows some of the metabolic processes that lead to cell death.
- Reduces use of oxygen and glucose by the brain.
- Should be initiated ASAP for at least 72 hours.
Journal of Perinatology 39 (2019)
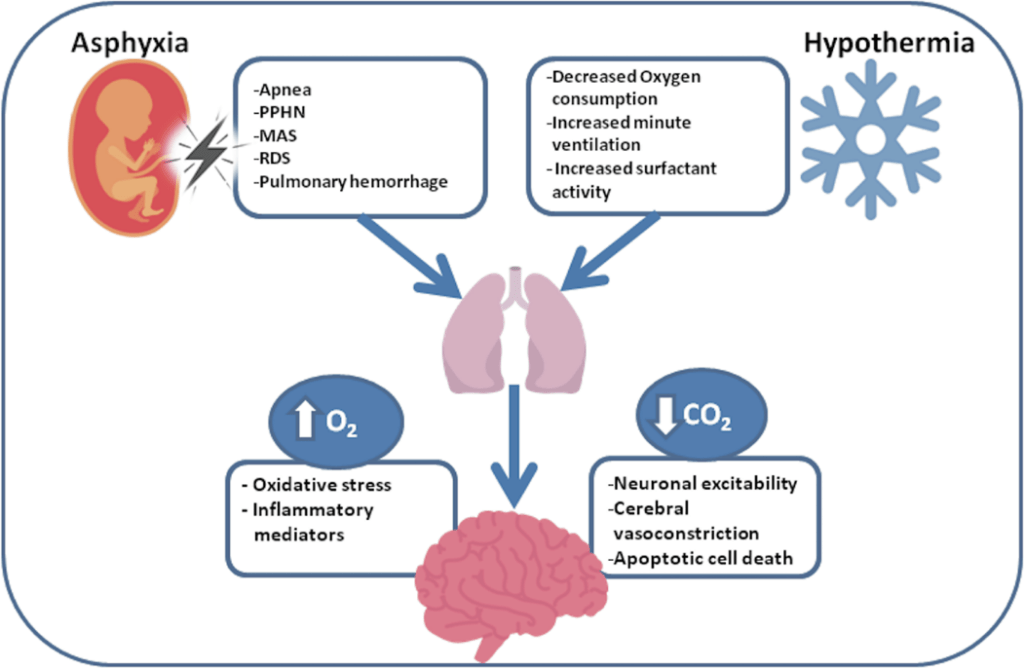
Managing Ventilatory Support: to avoid further hypoxia and prevent pulmonary hypertension as a result of asphyxia.
- Nitric oxide may be needed to assist with this.
- Avoiding hyperoxia which can lead to increase free radicals and injure brain further.
Prognosis:
Varies depending on initial injury. Mortality can be as high as 80% in sever insults. Seizures are common and their presence in Phase II portends a poor outcome. Loss of sleep-wake cycle portends poor outcome on EEG.
References:
Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective
Regan E. Giesinger, MD, et.al J Ped 180:22-30
Respiratory management during therapeutic hypothermia for hypoxic-ischemic encephalopathy
Eniko Szakmar, Agnes Jermendy, Mohamed El-Dib Journal of Perinatology (2019) 39:763–773
Antepartum and Intrapartum Factors Preceding Neonatal Hypoxic-Ischemic Encephalopathy
Miriam Martinez-Biarge, MD,et.al. www.pediatrics.org/cgi/doi/10.1542/peds.2013-0511
A case-control study of hypoxic-ischemic encephalopathy in newborn infants at >36 weeks gestation
Breda C. Hayes, MD,et.al. Am J Obstet Gynecol 2013;209:29.e1-19.
Predicting outcome in children with hypoxic-ischemic encephalopathy
Nicholas S. Abend, MD; Daniel J. Licht, MD Pediatric Crit Care Med 2008 Vol. 9, No. 1
Hypothermia for the treatment of infants with hypoxic–ischemic encephalopathy
RH Pfister and RF Soll Journal of Perinatology (2010) 30, S82–S87.
HYPOXIC-ISCHEMIC ENCEPHALOPATHY IN INFANTS: NEW CHALLENGES
Maria Gieron-Korthals & José Colón Fetal and Pediatric Pathology, 24:2,105-120
Current and Emerging Therapies in the Management of Hypoxic Ischemic Encephalopathy in Neonates
Jayasree Nair ID and Vasantha H.S. Kumar Children 2018, 5, 99




