By Santa J. Bartholomew M.D. FAAP, FCCM
Headache known as pain above the orbitomeatal line is one of the most common complaints in children and young people. The prevalence of headaches increases with age and greatly impacts school attendance for the child and work attendance for parents. The primary concern for caregivers always being brain tumor. Headaches are estimated to occur in 75% of adolescents and 25% of younger children with migraine being the most common reason for a child to see a neurologist.
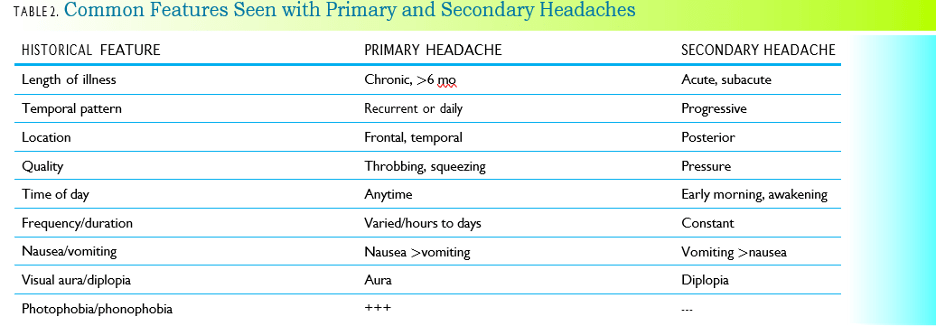
Thorough headache history and focused neurological examination are critical in evaluating headaches and distinguishing between primary headaches such as migraine, tension and chronic daily headache and secondary headaches such as those that occur with brain tumors, other causes of intracranial hypertension such as pseudotumor cerebri, meningitis, hydrocephalus from any cause. Acute febrile illnesses can also cause headache and essential hypertension. Classification of headache disorders have been established by the International Headache Society in 2013 and following these guidelines can help practitioners arrive at appropriate treatment plans for the particular headache the child is suffering from.
Getting a Headache History
- History needs to be gotten from parent AND child. Of course, questions need to be developmentally appropriate.
- Essential information in headache history
- When did headaches first begin?
- Location of the pain.
- Quality of the pain.
- Severity of the pain, has the pain remained the same or getting worse.
- Are there other symptoms such as focal weakness, sensory or visual disturbances, vomiting, light intolerance, double vision?
- Are headaches chronic or episodic? Frequency and duration of headache?
- How long have headaches been occurring?
- If headaches are long-standing has there been a change in the quality or position of the headache?
- Can you tell the headache is coming on?
- Has the headache every woken you up at night?
- Have you ever had a seizure with the headache?
- Are there activities or foods or medications that make the headaches worse?
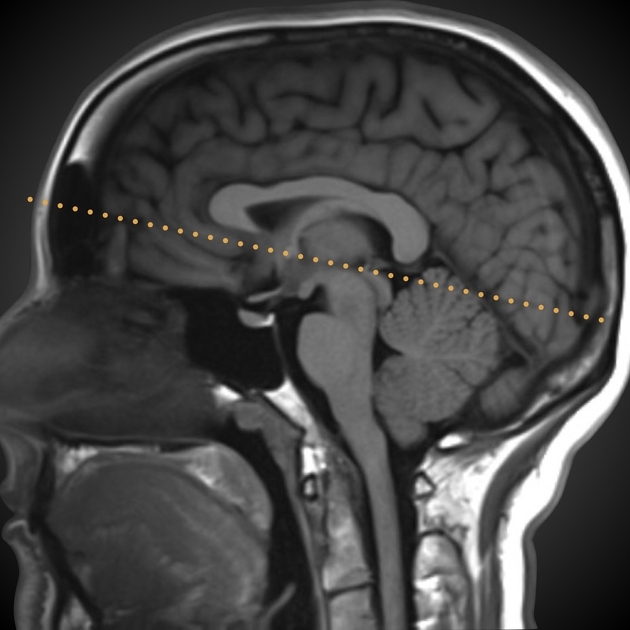
The Orbitomeatal Line
Focused Neurologic Examination
Although there is consensus on how to achieve historical data about history of headache through the International Headache society and the use of tools such as the Pediatric Migraine Disability Assessment (PesMIDAS) there is little consensus on the evaluation of these complaints.
- Assessment of the immunocompetence of the child
- Fever
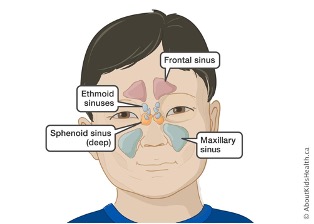
- Careful cranial nerve examination: nuchal rigidity, swelling of scalp, sinus tenderness, TMJ tenderness, posterior neck pain (sometimes seen in Chiari malformation), thyromegaly, muscular tightness.
- Palpation of head and neck:
- Assessment of gait and reflexes
- Careful examination of spine
- Careful examination of skin looking for signs of neurocutaneous disorders such as tuberous sclerosis. Neurofibromatosis.
- Assessment of the retina with full visualization of the optic nerve
- Auscultation of eyes, neck and head for bruits
- Assessment of oropharynx looking for tooth decay or tonsillar abscess
Diagnostic studies:
- Neuroimaging: may be considered when headache is subacute but rapidly progressive in severity, new onset of HA in immunocompromised child, presence of systemic findings like nuchal rigidity or fever, abnormal neuro examination in a new onset headache, headaches awakening a child from sleep.
- Neuroimaging should also be considered in all children WITHOUT a family history of primary headache disorders.
- EEG: not recommended in routine evaluation of headache in children as diagnostic yield is usually low.
- Lumbar puncture: not routinely recommended unless clinical presentation suggests infectious etiology to headache.
- Lab testing: often unnecessary in assessment of primary headache disorder unless there is suspicion of an underlying cause such as hyperthyroidism, severe anemia.
Primary Headaches
- Migraines:
- Intermittent attacks of headaches characterized by recurrent episodes of moderate to severe head pain lasting 2 to 72 hours.
- Usually, bifrontal or bitemporal
- Pain is usually focal, throbbing and worsens with activity.
- Can be accompanied by nausea, light sensitivity, and sound sensitivity
- 10% of children have an aura
- Treatment occurs in tiers:
- I: Analgesics such as Tylenol, Ibuprofen, Naproxen are the initial treatment for treatment naïve children
- II: Triptans: for children at least 5 years old and who have moderate to severe attacks. These are dosed by age, weight and ability to swallow a pill
- III: Multiple drug therapy: For children>5 years old who have refractory to monotherapy migraines. Suggestion is a tier I and II drug in combination.
- Chronic Migraine
- Migraine that occurs 15 or more days a month with at least 8 of the headaches having migraine features.
- More common in females than males.
- Overall prevalence in middles school to high school aged children is 1.5%
- Avoidance of overuse of medication is important step in prevention of chronicity.
- Tension Headaches
- Characterized by diffuse location, non-throbbing, mild to moderate in severity and does not worsen with activity.
- Typically last 30 min to 7 days and may be associated with light or sound sensitivity but symptoms do not include an aura, nausea or vomiting
- Acute treatment is with tier I drugs although gabapentin and Topamax have been used as medication alternatives.
- Prevention is accomplished with lifestyle modification: healthy habits such as not skipping meals, limiting caffeine consumption, good sleep hygiene.
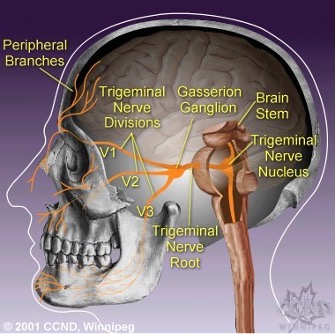
Cluster Headaches: constitute the most common trigeminal nerve headache. It is usually along the trigeminal nerve location.
- Pain is usually severe but lasts < than 3 hours. But multiple episodes of headache can occur during that time.
- They are often one-sided and in addition to headache the sufferer may have watery eyes, injection of the conjunctivae, runny nose or congestion, facial and forehead sweating, eyelid edema or droopy eyelid and changes in pupil response.
- Acute therapy includes: oxygen in an ED or urgent care setting or SQ sumatriptan or in patients who cannot administer an injection then IN sumatriptan.
- Patients who do not respond to these simple therapies may be treated with intranasal lidocaine of oral ergotamine’s
- Prevention should be initiated immediately for cluster headaches, and this includes preventative therapy with Verapamil or in active clusters glucocorticoids may help.
- Lithium and Topamax have also been used in combination with other drugs for refractory headaches.
Secondary Headaches
Headaches caused by an underlying condition.
- Acute febrile illness
- Rhinosinusitis
- Meningitis: acute or chronic
- Encephalitis
- Post-Traumatic headaches
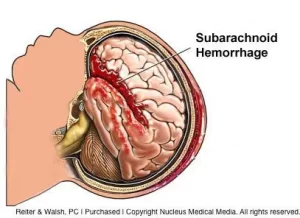
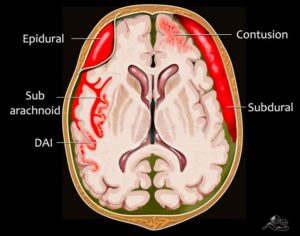
- Intracranial hemorrhage from trauma: epidural, subarachnoid or subdural hematoma
- Concussions
- Side effect of medications
- Headache medication overuse
- Severe and acute systemic hypertension (very high blood pressure)
- Brain tumor
- Idiopathic Intracranial hypertension: pseudotumor cerebri
- Hydrocephalus
In these cases head history usually sorts these patients from primary headache sufferers and physical examination provides clues to etiology of headache for example changes n mental status or gait disturbances, abnormal fundoscopic examination.
Diagnostics: imaging often is needed and helps identify the cause of the headache and when cause is identified then treatment can be determined.
References:
Popova V, Berk T Pedatric Migraine- An Updated Review. US Neurology.2019:15(2):68-73
Klein J, Koch T. Headache in Children. Pediatrics in Review 2020:41(4):159-169
Al Khalili Y, Chopra P. Migraine Headache in children Stat Pearls Jan 2022
Bonthisu D, Hershey A. Headache in Children: Approach to Evaluation and General Management Strategies. UpToDate Feb 2021
May A. Cluster Headache: Treatment and Prognosis. UpToDate Feb 2022
May A. Culster Headache: Epidemiology, Clinical Features and Diagnosis UpToDate Jan 2022
Wald E. Acute Bacterial Rhinosinusitis in Children: Clinical Features and Diagnosis UpToDate Nov 2022
Kacperski J, Kabbouche M, O’Brien H., Weberding J. The Optimal Manamgent for Heaches in Children and Adolescents. Ther Adv Neuro Dis 2016:9(1):53-68.