By Santa J. Bartholomew M.D. FAAP, FCCM
For newborns with congenital heart disease, early recognition and emergency stabilization and transport to a quaternary care pediatric center is essential. Cyanosis is a bluish color of the skin and tissues of a newborn infant. It occurs when the absolute level of reduced hemoglobin is more than 3-5 mg/dl. Cyanosis can be hard to evaluate in dark skinned infants making pulse oximetry in the newborn essential. Other physiologic factors can also affect cyanosis in the newborn such as hypothermia, high levels of fetal hemoglobin, alkalosis and low levels of 2,3 DPG (diphosphoglycerate).
Non-Cardiac Causes of Cyanosis:*
Cardiac Causes as Described by the Acronym “The 6 Tt’s”
- Meconium aspiration in the newborn period
- Newborn respiratory distress syndrome
- Neonatal pneumonia
- Pneumothorax
- Diaphragmatic hernia and other disorders of the diaphragm, airway, or lung structures
- Persistent pulmonary hypertension
- Shock in the newborn
- Acrocyanosis
* will be discussed in a separate article
- Transposition of the Great Arteries (TGA)
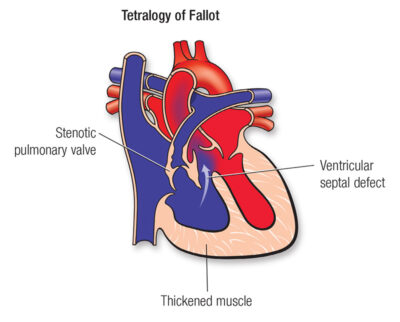
- Tetralogy of Fallot (TOF)
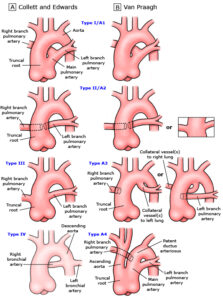
- Truncus Arteriosus (TA)
- Total Anomalous Pulmonary Venous Connection (TAPVC)
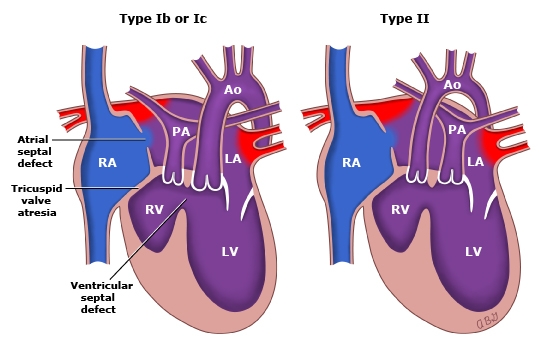
- Tricuspid Valve Anomalies (TA)
- “Tons of other lesions” such as DORV (double outlet right ventricle), multiple variations of single ventricles, HLHS (hypoplastic left heart syndrome), syndromes associated with hetrotaxy syndrome and anomalous venous connections.
Images of Lesions
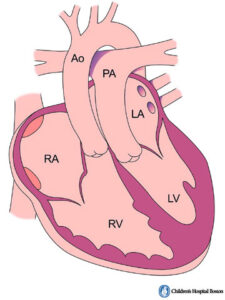
Central cyanosis of the infant occurs when blood shunts right to left across the ductus arteriosus (PDA) which is the blood vessel used to oxygenate the infant inside the mother. In utero this vessel helps shunt blood away from the lungs and oxygenation of the infant occurs via the placenta. When the baby is born, and they take their first breath the pressure in the lungs falls and blood begins to flow to the lungs and the PDA begins to close. This closure does not occur completely for a couple of weeks after birth.
There are heart lesions that are so severe that they cause cyanosis of the newborn with the ductus arteriosus open, the cyanosis is independent of the patent ductus arteriosus. These include TAPVC, TA and TOF (may or may not be dependent on PDA). These children can be placed on oxygen in the nursery and have no increase in their oxygenation. In these newborns it is a medical emergency for them to be transported to a cardiac center to provide mixing between the left and right side of heart which must be done in cardiac catherization lab or in the operating room to avoid death.
Lesions that are ductal dependent mean that when the ductus arteriosus is open there is sufficient mixing of left and right heart that the infant can survive for short period of time if the duct remains open. These lesions include HLHS, Critical AS, CoA, interrupted aortic arch, TOF with pulmonary atresia, pulmonary atresia with intact ventricular septum.
Newborns with cyanotic heart lesions often have difficulty with feeding, feedings that take extremely long time or resting between sucking, frequent choking or gagging, fast breathing, poor weight gain, irritability, excessive sleeping, persistent pallor.
Diagnostic Approach
- Physical examination: infants may have abnormal precordial activity, abnormal heart sounds, single or split-second heart sound and pathologic murmurs. In the abdomen they may have hepatosplenomegaly, diminished or absent pluses in the lower extremities and large variations in blood pressures between the arms and legs.
- Universal Pulse Oximetry: right hand normal and all other extremities low.
- CXR: cardiomegaly, abnormal cardiac silhouette, abnormal pulmonary markings.
- Hyperoxia test: has not been used as much any more since ECHO is so available but putting the child on 100% and testing oximeter to see if oxygen saturation increases.
Treatment in the Community Hospital
When a blue infant is identified that was not identified on fetal ECHO hyperoxia test may be useful to determine cyanotic heart disease vs non-cardiac heart disease. When cyanotic heart disease is a concern then keeping the ductus arteriosus patent is essential. This can be done medically with the use of prostaglandin infusions while awaiting transport. It is essential to identify these infants before leaving the nursery or at the very latest at the 1-week visit. After the ductus closes many of these children will present in shock and their morbidity and mortality increases dramatically.




