By Santa J. Bartholomew M.D. FAAP, FCCM
Acute Abdominal Pain in Children: Surgical Emergencies
Abdominal pain in children is a very frequent complaint. Physicians must determine from the myriad of these complaints which 2% of children have catastrophic abdominal issues. And because many of these complaints are mostly benign it is quite easy to be lulled into complacency and miss a child with catastrophic abdominal problems. Assessing abdominal pain requires exemplary clinical acumen and a constant index of suspicion for an acute serious problem causing the abdominal pain.
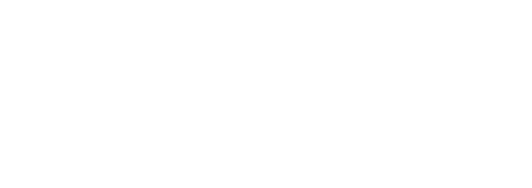
Causes for Abdominal Pain
Causes of abdominal pain differ by age group and is extensive. The table below shows the most common causes in each age group.
Abdominal pain is perceived by two sets of pain receptors:
- One set on the mucosal lining of the bowels, and
- The other on the serosa or fibrous lining of the abdominal cavity.
Pain is usually poorly localized until the serosal surface becomes inflamed such as in appendicitis, then pain is easier to pinpoint to a specific area. Despite this inflammation however, children younger than 5 years old will have difficulty localizing pain.
Most abdominal pain is self-limiting and not life threatening: 48% of abdominal pain is constipation, 19% is left undiagnosed and only 2% of abdominal pain has a surgical cause. So diagnosis can be likened to a needle in a haystack but organized and methodical evaluation usually leads to appropriate diagnosis.
Making The Diagnosis
- Detailed and careful history including not only the history of the present illness but past events and medical history; complete family history of abdominal diseases.
- Thorough physical examination including digital rectal examination.
- Focused laboratory examination based on differential diagnosis for the age group of child.
- Focused radiographic examination based on differential diagnosis for the age group of child: ultrasound has gained great popularity as it does not require sedation in young children and does not expose children to large amounts of radiation. The usefulness of US in obese or very uncooperative children may make this modality difficult.
- CT remains the gold standard imaging study for many abdominal processes such as appendicitis and volvulus.
- MRI is becoming more popular but often requires sedation for younger children.
Abdominal Emergencies
Midgut Volvulus
Midgut volvulus is a twisting of the bowel that can cause lack of blood flow to the bowel from a few minutes after the twist. Bowel become quickly necrotic if not untwisted urgently. Children can lose part to all their bowel causing them to have short bowel syndrome and not be able to eat by moth for the remainder of their life.
- One must have a high index of suspicion to make this diagnosis which is done by upper GI.
Appendicitis
Appendicitis is the most common surgical emergency in childhood although unusual in children under 5 years old. It is an inflammation of the distal end of the cecum and can progress from inflamed to perforated in under 12 hours causing severe sepsis and death if not treated quickly.
- In 35% of cases a fecolith (hard piece of stool) is found to obstruct the lumen causing subsequent inflammation.
- How does this happen? See Fig. 2
- Recent development of scoring systems have largely superseded radiographic tests but US and CT are still useful in difficult diagnoses. See Fig. 1
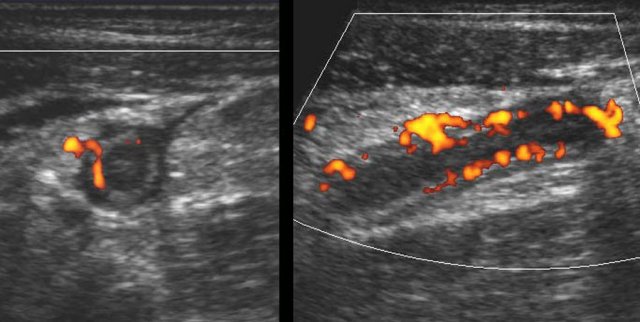
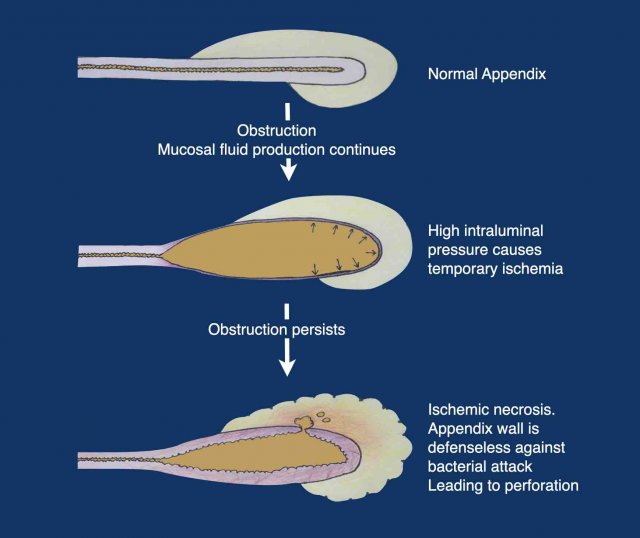
Figure 1. Large thick-walled inflamed appendix by ultrasound
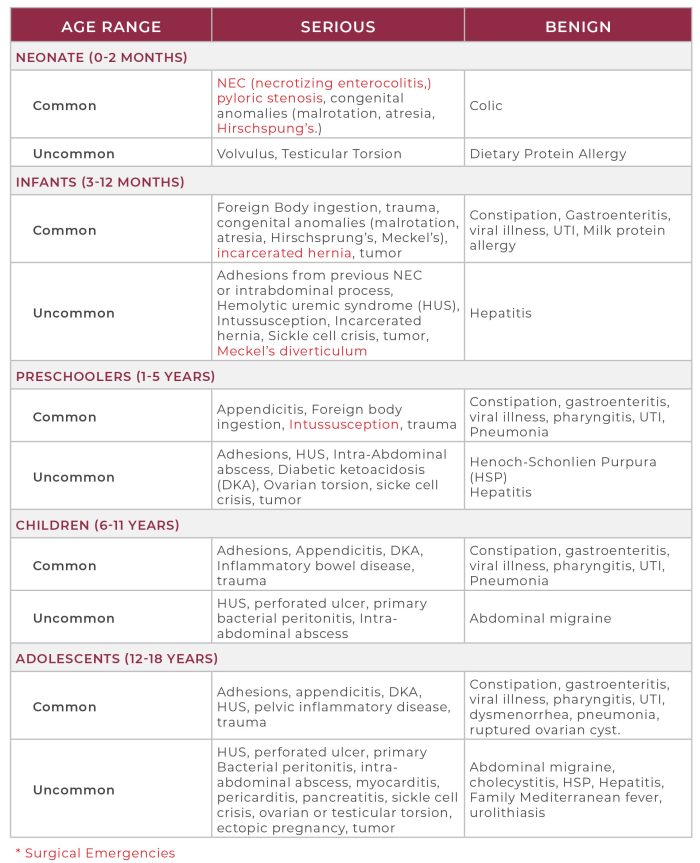
Intussusception
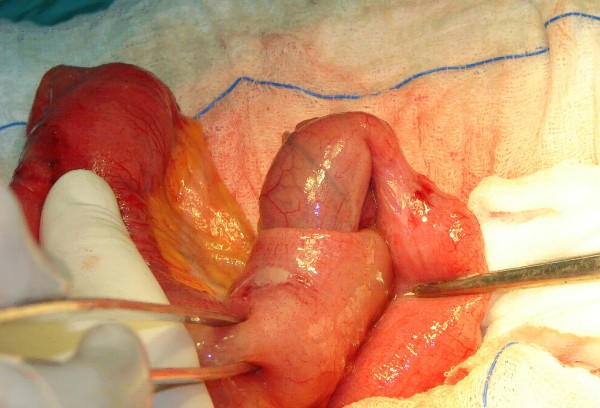
Intussusception is an invagination of the proximal segment of bowel into the distal segment of bowel (See Fig. 3) as this happens the mesentery (which contains vasculature) is dragged with bowel causing it to become ischemic, swollen and possibly having the bowel perforate.
- Children usually present with severe abdominal pain, sausage shaped mass in abdomen and currant jelly (reddish black) stools. See Fig. 4
- Children are listless and septic appearing.
- The lead point for the intussusception can be a variety of things: Meckel’s diverticulum, patches of lymph tissue known as Peyer patches, there is also an increased risk with rotavirus vaccination.
- Ultrasound has been revolutionary in early diagnosis and usually these can be reduced in radiology without surgical intervention with the use of contrast enema’s.
- Chance of success with this method depends on the time the bowel has been intussuscepted, the age of child, and if there is a lead point.
- Unstable patients go directly into surgery for reduction otherwise stable children can undergo multiple attempts at reduction in radiology.
- Perforation occurs in <1% of children.
- Children are listless and septic appearing


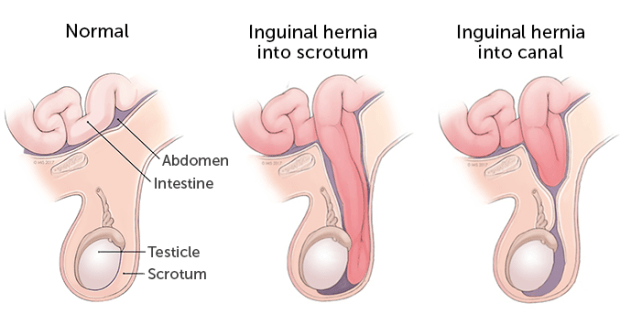
Incarcerated Hernia
Incarcerated hernia is when the bowel slips through an opening in the abdominal musculature into the scrotum or labia major and it cannot be gently pushed back into place. This causes the bowels blood flow to be compromised hence the bowel can die causing sepsis in the child.
Surgical reduction of the bowel or resection of the bowel and the repair of the abdominal wall defect prevent further episodes of damage.
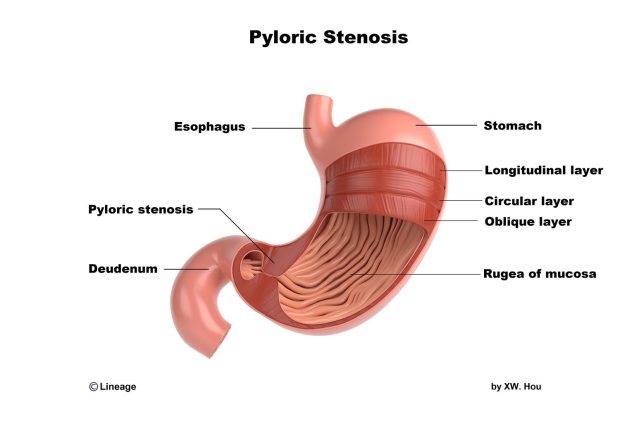
Pyloric Stenosis
Pyloric Stenosis is a hypertrophy of the muscle at the outlet of the stomach that causes narrowing of the outlet of the stomach into the small bowel that causes persistent vomiting in the infant and profound metabolic abnormalities in the blood in the first few weeks of life because formula cannot pass through to small bowel.
- Usually diagnosed by Ultrasound or upper GI.
- The cure for this is making an incision in the muscle and opening the outflow tract of the stomach.
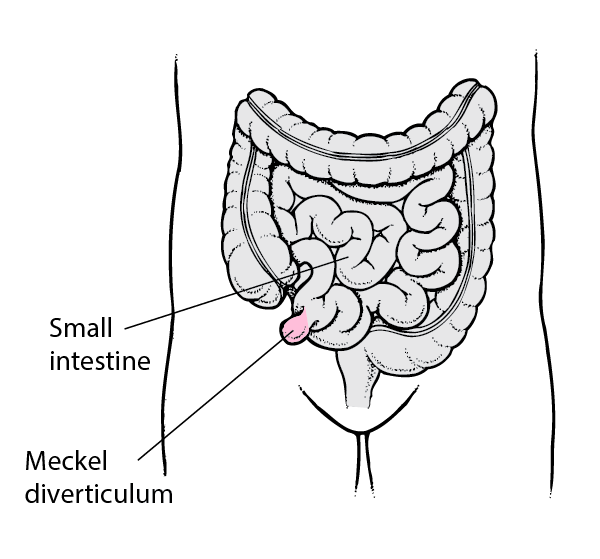
Meckle’s Diverticulum
Meckel’s diverticulum is an out pocketing of the end of the small bowel that is a congenital abnormality found in about 2% of the population of which up to 60% of which contain gastric tissue.
- Typically painless but can cause minimally painful rectal bleeding, abdominal distension and vomiting.
- Can also ulcerate and perforate or present as the lead point for intussusception.
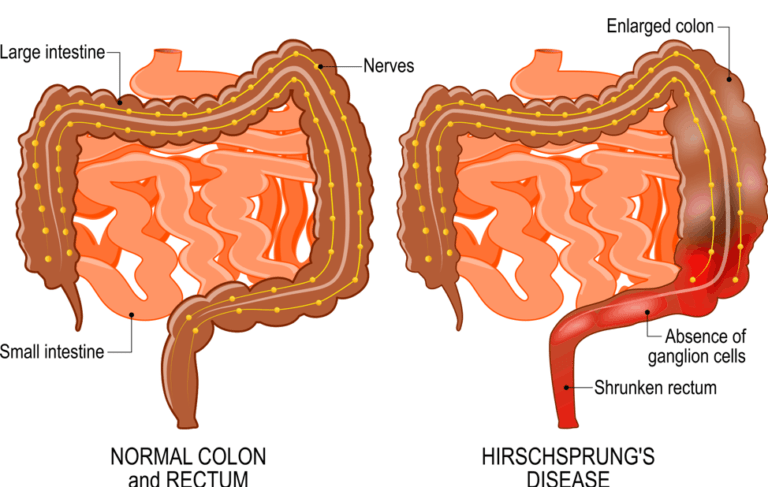
Hirschsprung’s Disease
Hirschsprung’s Disease is characterized by lack of ganglion cells in the distal gut making movement of stool through the bowel very difficult.
It is the most common gut motility disease in children. Suspected in infants with difficulty stooling and abdominal x-rays with hugely enlarged colon.
- Diagnosis is made by rectal biopsy.
- Treatment begins with rectal washouts and dilations of the rectum and then is completed with an endorectal pull through procedure – which pulls bowel through and resects the affected portions leaving healthy bowel remaining.
Testicular Or Ovarian Torsion Testicular
Testicular torsion occurs when a testicle rotates, twisting the spermatic cord that brings blood to the scrotum. The reduced blood flow causes sudden and often severe pain and swelling. Testicular torsion is most common between ages 12 and 18, but it can occur at any age, even before birth.
- Age distribution is bimodal with a peak in the neonatal period and a peak in puberty.
- Newborn testicular torsion can present as painless scrotal swelling and the salvage rate is very poor, approximately 9%. This is thought to be secondary to poor fixation of the neonatal tissues to one another. It is predominantly an extra-vaginal torsion – this accounts for 5% of all torsions.
- Occurs more frequently in high birth weight infants.
- Scrotal imaging can aide in diagnosis
Older Children and Adults Testicular Torsion
- Testicular torsion or acute scrotum is heralded by a sudden unbearable unilateral scrotal pain in the scrotum.
- Patients may have
- Fever
- Nausea
- Vomiting
- Generalized abdominal pain
- Higher testicular position – indicative of a twisted and shortened spermatic cord.
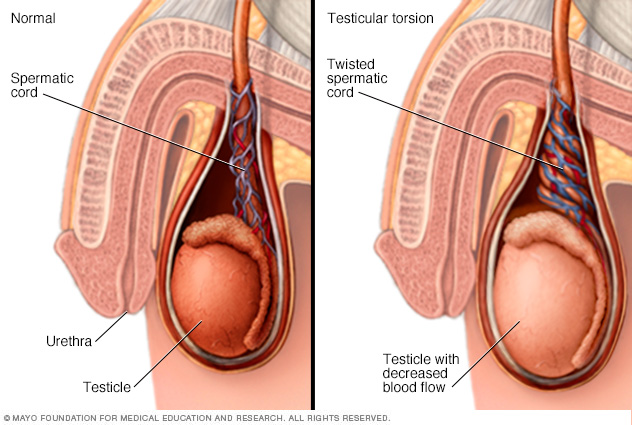
Acute scrotal pain must be evaluated quickly as it is a surgical emergency to try to untwist and save the testicle. For this reason, any adolescent that complains of abdominal pain should always have a scrotal examination as part of their evaluation. Every 10 minutes of delay in releasing the torsion testicular survival is diminished by 5%.
Testicular examination can be summarized by the scoring system known as TWIST, short for Testicular Workup for Ischemia and Suspected Torsion.
Parameters include:
- Swelling of the scrotum and testicles –
where normal landmarks (epididymis) may not be palpable due to swelling (2 pts) - Hard testicle (2 pts)
- Absent cremasteric reflex (1 pt)
- Nausea/vomiting (1 pt)
- High raised testicle (1 pt)
- Risk is assessed as
- low (0-2 pts)
- medium (3-4 pts)
- high (5-7 pts)
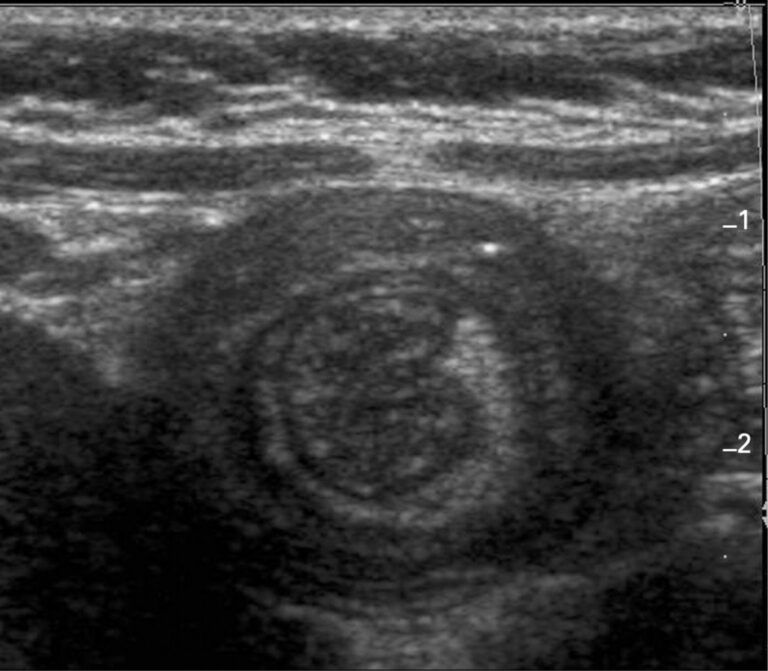
Ultrasound can be used to confirm diagnosis: typically reveals a whirlpool sign. See Fig. 5 It is possible to provide analgesia and try manually un-twisting, but more often these children are taken to the OR for decompression.
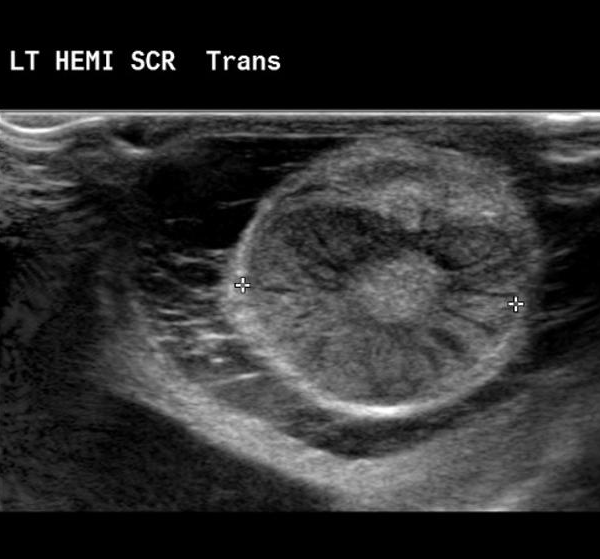
Figure 5. Testicular Torsion by Ultrasound
Ovarian
Ovarian torsion is a rare issue in pediatrics but must be included in any differential of abdominal pain in a female child or a child with an abdominal mass in the premenarchal or preteen years.
Clinical presentation is non-specific so diagnosis relies on a high index of suspicion. Most common symptoms are:
- Lower abdominal pain,
- Nausea, and
- Vomiting.
- Some children also report flank and back pain.
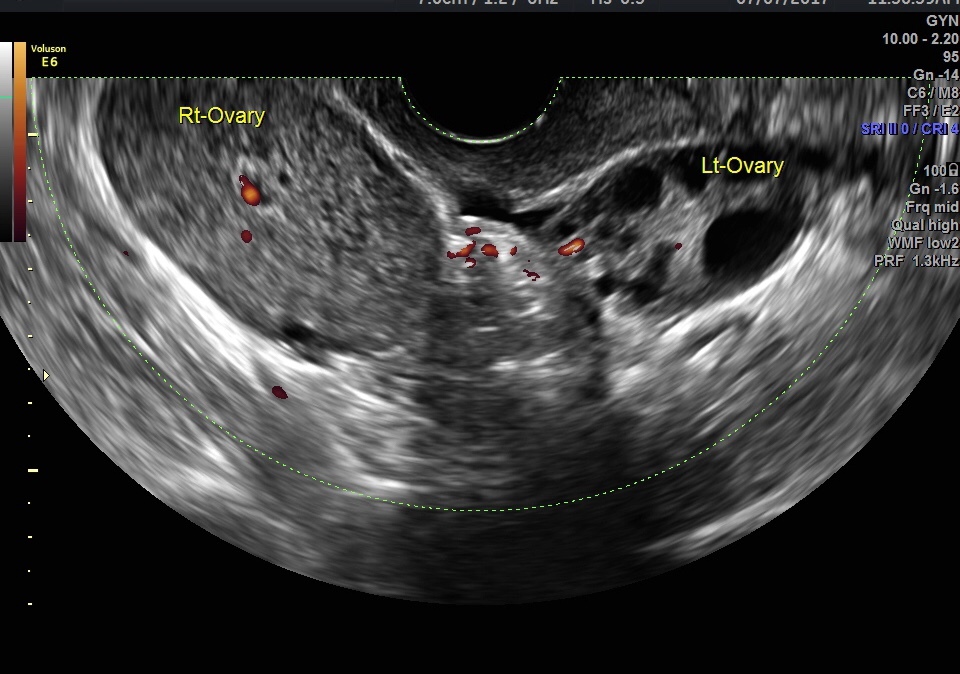
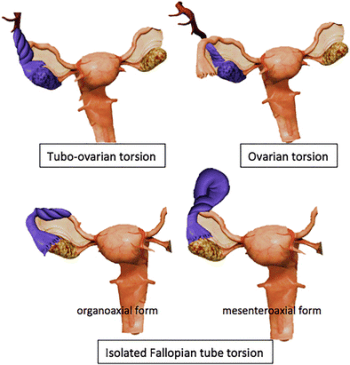
Ultrasound is the most useful way of evaluating these children (See Fig. 6) to visualize the ovary and possible torsion of it. In cases of ovarian torsion it is common to find an ovarian cyst or benign teratoma. Ovarian pathology in torsion cases is found in 50% to 84% of cases.
Treatment is operative.