By Santa J. Bartholomew M.D. FAAP, FCCM
Intentional burns are a serious form of child abuse that can cause long-term health issues and harm. Approximately 70% of children who get admitted to hospitals with burns are younger than five years old and these burns are scald burns. This developmental age range is particularly at risk as they are beginning to explore their environment with no cognitive awareness of the dangers that exist in the household: electric sockets, hot liquids on the stove, glass covering gas fireplaces, stoves, and the like.
A smaller portion of these burned children are victims of true neglect and abuse. An estimated 24% of the burns are suspected to be abusive. Burns are a very important cause of injury in children being the third most frequent cause of injury resulting in death behind motor vehicle accidents and drowning. It is paramount to discover their etiology to prevent further injury in neglect and abuse situations
Burn Types
Predominant burn types were scald burns (40% of these burns hot water), then contact burns, chemical burns, and friction burns in decreasing order. The most common sites of abusive burns in decreasing order are legs, buttocks/perineum/genital area, and trunk. Immersion burns are by far and away the most common and significantly more likely to be abusive in origin.
Approximately 70% of children who get admitted to hospitals with scald burns are younger than five years old.
Intentional burns usually present in sharp margins from a child being held in hot liquid without the splash marks seen more frequently in accidental burns. Intentional scalds tend to be uniform and have a 360-degree involvement. There may be spared areas where a body part was against the bottom of the container or the child was held in such away that areas of skin did not come in contact with hot liquid.
Hot water, the most common liquid for immersion can cause partial and full thickness burns:
- in 1 second at 156°
- in 2 seconds at 149°
- in 5 seconds at 140°
- in 15 seconds at 133°



When evaluating these children, physicians and law enforcement need to ask themselves “Does the story fit the explanation?” For example, the photos above may have come with the explanation: “The child was in the tub/sink and turned on the hot water!”
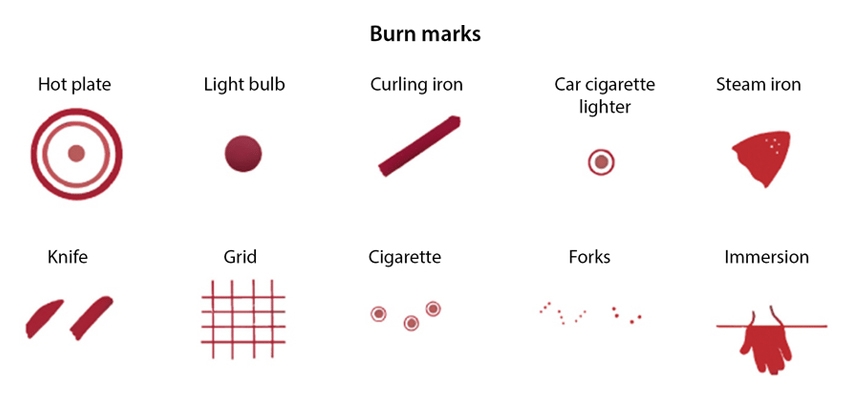
Contact burns, such as with curling irons, furnace grates, irons, stoves, oven doors, and cigarettes are common in small children. Accidental burns are more likely to exhibit unclear margins, as the child is trying to escape the object. If an object fell onto the skin, such as when a child pulls on an iron cord, the burn will likely exhibit an unclear margin as the iron briefly hit the skin. Many times, contact burns are seen on the palm of the hand due to the child grabbing the object. Intentional burns can also be caused by the above objects, but are likely to reveal a clearer pattern, have distinct margins, and may occur on areas normally covered with clothing.
The motivations and risk predictors for such horrific acts are interrelated, with acute family stress and lack of external support powerful precipitants of intense frustration and compounded in low-income, single-parent families of multiple children. Abuse is symptomatic of dysfunction and the origins of such behavior in the abuser stem from poverty, desperation, substance dependence, and potential previous abuse. Frustrations often overcome the abusers’ emotional reserves, especially with small children who are at their most demanding and are also easy targets for maltreatment. Frustrations are often vented as children can precipitate acute stress during periods of increased maintenance requirements such as toileting.
Close and careful attention to the assessment of etiology and the family dynamic are an absolute necessity in keeping children safe.




References:
Scald Statistics and Data Resources ABA conference slides Feb 3-9, 2019
Peck, Michael. Epidemiology of Burn Injuries Globally Up-to Date 2021
Pawlik, Marie-Christin, et.al. Children with burns referred for child abuse evaluation: Burn characteristics and co-existent injuries Child Abuse & Neglect 55(2016) 52-61




